
Osteochondrosis is a degenerative-dystrophic lesion of the spine, which leads to the destruction of the intervertebral discs with the corresponding consequences. Osteochondrosis "infects" the entire spine, but the symptoms of the disease are more pronounced when the cervical region, as the most mobile, and the lumbar region are affected. The thoracic region is the one that suffers the least.
The signs of osteochondrosis of the neck are very diverse and often resemble other diseases, which makes differential diagnosis and early recognition of the pathology difficult. In this article we will look in detail at how osteochondrosis of the cervical spine manifests itself and what will help you suspect this disease.
Degrees of osteochondrosis.
Osteochondrosis is a chronic progressive disease that occurs with periods of remissions and exacerbations. Pronounced clinical symptoms do not appear immediately, but after some time, when the degenerative process enters the second or even third stage.
There are only 4 degrees of pathology:
- The initial stage is characterized by pathological changes within the intervertebral disc. It loses moisture, which causes degenerative changes, decreased disc height, and cracking of the fibrous capsule. As a rule, at this stage there are no signs. Diagnosis is only possible through an MRI of the spine. This is the most favorable stage for starting treatment, since in this case it is possible to completely restore damaged discs, which cannot be done in the future.
- Osteochondrosis of the second degree is characterized by worsening damage to the intervertebral discs. Its height decreases significantly, which causes sagging of the muscles and ligaments of the spine. All this causes instability of the damaged segment of the spine, increased mobility of the vertebrae, their displacement and sliding relative to each other and with the spinal axis. As a rule, it is at this stage that the first signs of the disease appear in the form of pain and other specific signs of injuries to the cervical spine.
- In the third stage, bulges and herniations of the intervertebral discs develop. The symptoms of the disease are fully expressed.
- The fourth stage is the last. In this case, the formation of osteophytes and spinal deformities occurs. The body tries to somehow stabilize the damaged segment of the spine, so osteophytes, ossification of ligaments and other processes develop that lead to stabilization of the vertebrae, but, unfortunately, this process is accompanied by vertebral subluxations and various types and degrees of spinal deformities.

The nature of the symptoms of cervical osteochondrosis.
Manifestations of osteochondrosis in the cervical spine are associated with 3 mechanisms of the negative impact of this pathology:
- Direct compression of the spinal cord, which runs through the spinal canal. It should be noted that this occurs very rarely with an advanced degenerative process and its complications. Compression of the nervous tissue of the spinal cord can be caused by a large intervertebral hernia, which protrudes directly into the lumen of the spinal canal; stenosis (narrowing) of the spinal cord canal due to degenerative changes; Dislocations, subluxations, fractures of damaged vertebrae.
- Negative effect on the structures of the peripheral nervous system (spinal cord roots and nerve fibers) leaving the cervical spine. They may become compressed between adjacent vertebrae or hernial protuberances and may become inflamed and irritated. All this leads to a series of serious symptoms. This is the most common group of signs of cervical osteochondrosis.
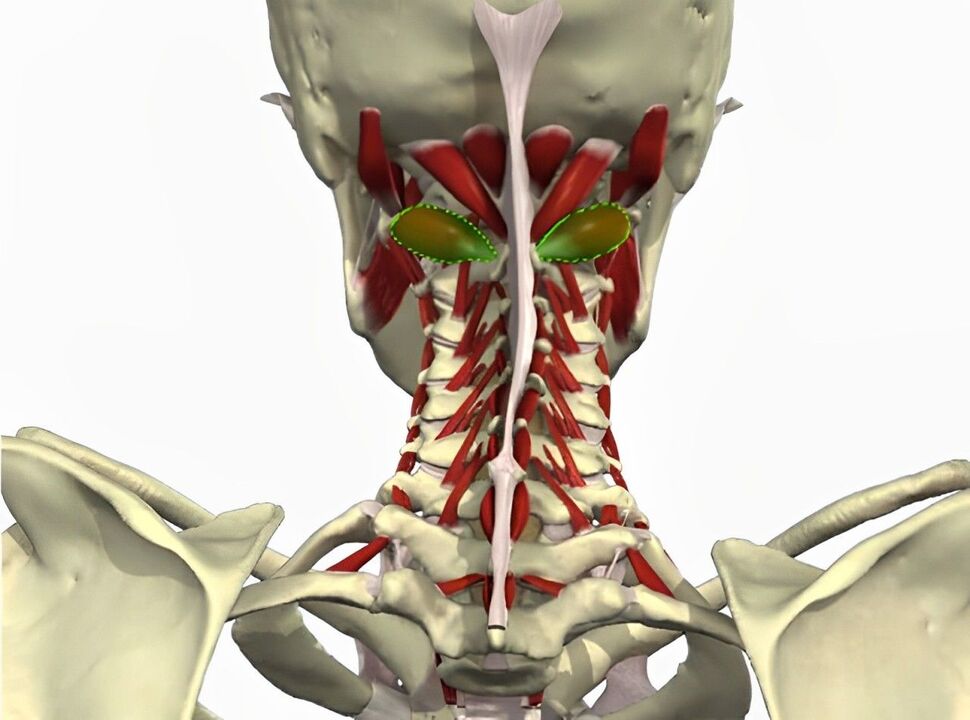
- Negative effect on blood vessels passing near the damaged area of the spine. In particular, a very important arterial vessel is of clinical importance - the vertebral artery, which passes through the openings of the transverse processes of the cervical vertebrae into the cranial cavity and supplies blood to the posterior third of the brain and the cerebellum.
Let's consider in detail each group of mechanisms and what symptoms they cause.
Symptoms associated with spinal cord injury
As already mentioned, spinal cord compression with cervical osteochondrosis is very rare. This is a very serious condition that can cost a person not only their health, but also their life.
Damage to the upper cervical spine is life-threatening. The cardiovascular and respiratory centers suffer, which leads to immediate death. With compression at the level of the 3-4 segment of the spinal cord, tetraplegia develops (paralysis of all limbs and muscles below the lesion). The respiratory muscles and diaphragm also suffer, which can lead to respiratory arrest and death.
If damage occurs at the level of segment 4-5 of the spinal cord, tetraplegia develops, but without respiratory failure. When 5 to 8 segments of the spinal cord are compressed, several muscle groups of the upper extremities suffer and paraparesis of the legs and disruption of the pelvic organs occur.
Symptoms associated with nerve damage.
pain syndrome
First of all, it is worth highlighting the pain syndrome, which can be chronic (cervicalgia) and acute in the form of lumbago (cervicalgia). Pain occurs in the neck, occipital part of the head and shoulder girdle. It is usually caused by irritation, compression and inflammation of the nerve roots of the cervical spine, as well as pathological spasms of the muscles in this area, which are innervated by these nerves.
The pain associated with neck pain is almost constant, painful and varies in intensity. As a rule, the pain syndrome can be tolerated. It appears or intensifies with sudden movements, turns and tilts of the head. Neck movements are accompanied by a characteristic crunch.
Cervical pain occurs suddenly in the form of a gunshot or electric shock. It's very intense, it goes to one of the hands. It lasts a few seconds or minutes, then gives way to neck pain. It is usually caused by a sudden movement and compression of the nerve.

Root syndromes
All major nerves of the upper extremity (median, ulnar and brachial) are formed from nerve fibers emerging from the cervical spine. Therefore, in the presence of cervicobrachial osteochondrosis, these nervous structures may suffer. All of these nerves are mixed, that is, they have both sensory and motor functions. Depending on which root is affected, the symptoms will be different. For example, sensation in the second or third finger may be lost and paralysis of one or more muscles may occur. All of these signs of nerve damage are classified into separate syndromes, which only a neurologist can determine.
occipital neuralgia
Occipital neuralgia develops when the greater and lesser occipital nerves, which are made up of the second, third, and fourth pairs of cervical spinal nerves, are damaged. When these structures become compressed, irritated or inflamed due to a degenerative process in the spine, a headache occurs in the back of the head, which women often complain about.
This pain is so typical that only its description allows a correct diagnosis to be made in 90% of cases. It is also called stabbing cranialgia. A pain attack occurs suddenly, has a unilateral localization (it rarely hurts on both sides), patients compare the nature of the pain with an electric shock. The attack lasts several minutes, but can recur several times a day. The pain occurs on the posterolateral surface of the neck and extends upward to the occipital protuberance (repeats the anatomical course of the occipital nerve). At the same time, a sensitivity disorder may develop in the skin on the back of the head (numbness, tingling sensation).
cardiac syndrome
This name is due to the fact that this manifestation of osteochondrosis of the cervical spine is very similar to angina pectoris and other heart diseases. The reason for this phenomenon is damage to the nerve fiber innervating the pectoralis major muscle and the phrenic nerve, the fibers of which are woven into the pericardium of the heart.

The cause of pain is spasm of the pectoralis major muscle due to pathological impulses along the damaged nerve fiber. At the same time, patients often confuse this pain with heart pain. Unlike coronary pain, pain syndrome with cervical osteochondrosis has a long duration (sometimes several hours or days), which does not happen with angina pectoris, is not associated with physical activity, but is related to body position. The pain intensifies with sudden movements, turning the head, coughing, sneezing, which does not happen with angina. Antianginal drugs (nitroglycerin, etc. ) will not be effective.
Important! In any case, these symptoms require a thorough differential diagnosis, because atypical variants of angina and heart attack also occur. In order not to miss a serious illness, you must first perform an ECG. With osteochondrosis, pathological changes will not be recorded.
Symptoms associated with vertebral artery injury.
Compression of the vertebral artery during cervical osteochondrosis can provoke a large number of unpleasant manifestations, which are mainly associated with a decrease in blood flow and hypoxia of the part of the brain that is fed by this vessel (the posterior third of the brain and the cerebellum).
Signs of vertebral artery syndrome:
- headache of a diffuse or throbbing nature in the nape of the neck, temples and parietal region;
- dizziness;
- nausea and vomiting;
- visual disturbances;
- ringing in the ears, decreased hearing acuity;
- impaired coordination and balance;
- development of fall attacks (sudden falls without loss of consciousness due to sharp turns of the head);
- memory impairment, decreased performance, ability to concentrate.
Important to remember! With pronounced changes in the spine, the artery can be compressed so much that it will lead to the development of an ischemic stroke in the vertebrobasilar region of the brain. Therefore, it is important to suspect pathology in time and take all necessary measures to improve spinal health and prevent further pathological changes.
Frequently asked questions
What symptoms accompany cervical osteochondrosis?
Symptoms of cervical osteochondrosis may include pain and stiffness in the neck, headaches, dizziness, tinnitus, and tingling or numbness in the arms and shoulders.
How can the symptoms of cervical osteochondrosis be relieved?
To alleviate the symptoms of cervical osteochondrosis, it is recommended to exercise, maintain correct posture, avoid sitting for a long time in one position, use special pillows and mattresses, and also use physiotherapy methods.
Helpful tips
Tip #1
Pay attention to pain in the neck, shoulders and arms, which may be symptoms of cervical osteochondrosis. The pain can be sharp, dull, or localized to certain points.
Tip #2
Pay attention to numbness or weakness in the arms, fingers or shoulders, as this can also be caused by cervical osteochondrosis.
Tip #3
Pay attention to headaches, dizziness, and tinnitus, as these symptoms may also be associated with cervical osteochondrosis.












































